All published articles of this journal are available on ScienceDirect.
Mastalgia in Fibrocystic Changes; From the Diagnosis Bench to Innovative Therapy: A Narrative Review
Abstract
Fibrocystic breast change (FBC) is a prevalent benign breast condition that affects women of reproductive age. Hormonal fluctuation during the menstrual cycle is the suggested pathology. Affected women suffer cyclical breast pain (mastalgia), change of breast texture, and nipple discharge.
Multiple diagnostic and therapeutic approaches were used to address mastalgia in FCB; the last decade witnessed considerable advancement in therapeutic modalities, showing variable degrees of efficacy in alleviating mastalgia.
This review aims to examine recent data linked to FCB diagnosis, in addition to discussing and comparing the latest therapeutic options in FCB cases.
An online search was conducted via four major electronic databases using keywords related to FCB, pathology, imaging, and therapy. Data of interest were extracted and analyzed. Our findings indicate that mammography takes the lead in diagnosis, and ultrasound is complementary. Innovative bioinformatics holds promise in improving diagnostic precision and improving outcomes. Lifestyle changes remain the first therapeutic option, which was combined with drug therapy tailored according to the etiology and nature of pain with a varying degree of efficacy. Innovative therapeutic strategies were discussed, showing good efficacy, a low rate of side effects, and high patient acceptability. Empowering physicians with recent knowledge will refine diagnostic challenges, guide therapy choices, enhance patient outcomes, and allow holistically centered health care.
Future research is needed to explore optimal diagnostic follow-up approaches, added to best treatment combinations and newer therapies with better safety profiles and more patient satisfaction.
1. INTRODUCTION
Fibrocystic breast change (FBC), also known as diffuse cystic mastopathy, is a benign alteration in the breast functional unit (the lobule). FBC is not a distinct entity but rather a broad spectrum of altered breast morphology. It is one of the most prevalent benign conditions affecting women of reproductive age, typically between 20 and 50 years, with peak incidence occurring around perimenopause [1]. The breast tissue is typically composed of a mixture of glandular, fibrous tissues wrapped in fatty components (Fig. 1). In FBC, the fibrous tissue becomes abundant, and multiple cysts form that become filled with fluid. Finally, the breast duct enlarges and becomes more prominent, leading to increased cyst formation, fibrosis, and adenosis (Figs. 2 and 3). These changes alter the breast texture, making it lumpy and intermittently painful, particularly around menstruation [2]. FBC is most commonly observed in nulliparous women, those with low parity, individuals with a thin body figure, and cases undergoing estrogen hormonal therapy. Not all affected women exhibit symptoms; 50% of cases are symptomatic, while histological evidence of FBC is present in up to 90% [3]. The trigger for FBC is not well understood, but certain studies suggest that hormonal fluctuations during the menstrual cycle contribute to its development. In the late cycle, mitosis occurs, followed by apoptosis, both of which manifest in the breast as altered stromal or ductal tissue damage.
The use of exogenous hormone replacement therapy for women in menopause can perpetuate this alteration, which supports the hormonal theory [4].
Certain studies describe FBC as part of the aging process. In their twenties, women exhibit proliferative stroma (mastoplasia phase). Before the age of 35, breast tissue undergoes involution, characterized by microcyst formation and ductal changes. In their thirties, marked ductal hyperplasia and alveolar cell proliferation (adenosis phase) occur. By their forties, large tender cysts of varying sizes develop (cystic phase) [1].
Many studies have examined the complex pathophysiology of FCB and tried to define what triggers mastalgia among cases. A comprehensive review by Murshid KR et al. in 2011 [5] addressed most of these topics. However, significant advancements in the field warrant a fresh evaluation. This review aimed to incorporate recent developments in FCB diagnostic modalities with a critical appraisal of their cons and pros. Additionally, it will assess and explore recent improvements in therapeutic options and innovative therapeutic modalities that offer effective and sustainable patient improvement.
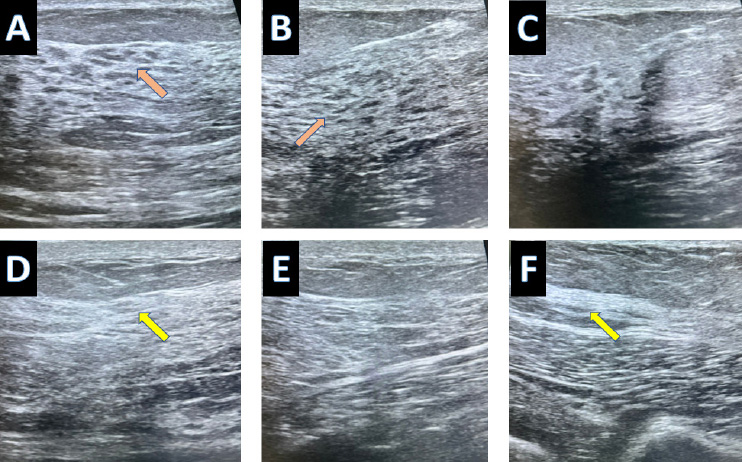
A normal breast ultrasound in a 23-year-old female showed glandular distribution (A, B, C) and normal fibrous tissue sounding the breast gland (D, E, F).
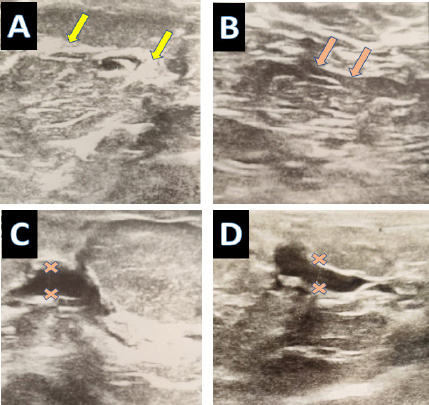
Typical fibrocystic changes in breast tissue are (A) Abundant fibrous tissue bands and (B) prominent thin wall ducts. Localized prominent ductal changes; (C) Thickened walls, dilated, irregular ectatic ducts that have internal echo-free contents suggesting intraductal proliferation and periductal inflammation; and (D) dilated ducts with adjacent microcytic changes.
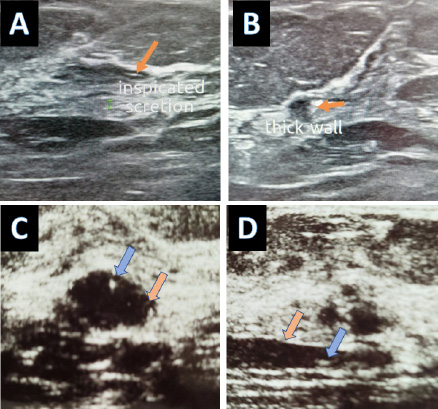
(A) Thin-walled ectatic duct with intraluminal inspissated secretion. (B) Thick wall ectatic duct with regional tubular duct ectasia suggesting mastitis (C) The ectatic duct resembles a cyst in a cross-section image (D) Longitudinal scan through duct ectasia showing internal echogenic debris; blue arrow.
2. METHODS
An online search was conducted using electronic repositories (PubMed, Scopus, WOS, and Google Scholar) to synthesize literature on FBC and mastalgia. Furthermore, to ensure methodological rigor and reporting quality, the SANRA guidelines for narrative review articles were followed. The review addressed justification, transparency in research methods, scientific reasoning and referencing, structured presentation, and critical appraisal of the results obtained [6].We expanded our search to include studies published in the last 2 decades until October 2024. The inclusion criteria were peer-reviewed studies that addressed the incidence, pathology, pathophysiology, diagnostic imaging modalities, and therapeutic options in FBC. No language restrictions were applied. Editorials, case reports, and papers addressing conditions outside the scope of our topic of interest were excluded.
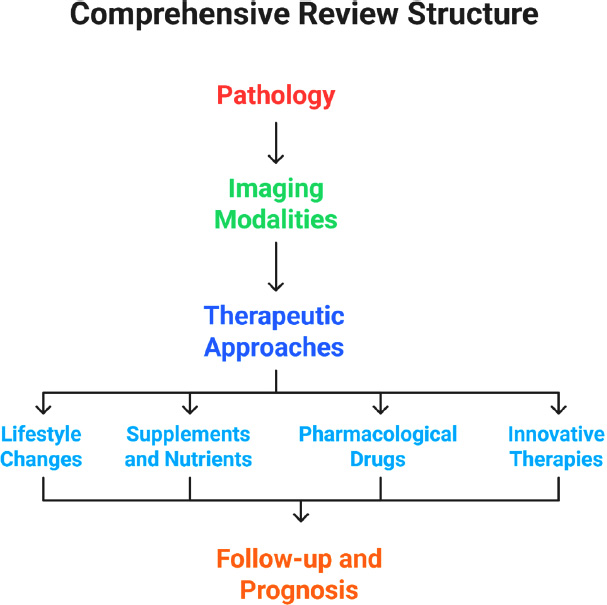
Two independent reviewers assessed the articles for eligibility, and disagreements were resolved by a third reviewer. Each article was evaluated for quality and reliability, considering sampling power, study designs, and confounders; Fig. (4) shows the study flowchart. The review was structured under the following subheadings:
2.2. Imaging Modalities
Includes the advantages, limitations, and role of diagnostic imaging in differentiating FBC from malignant pathology.
The study flow chart.
| Non-proliferative | Proliferative | Refs. |
|---|---|---|
|
Cystic changes • There are fluid-filled, round to-ovoid cysts lined by single columnar or cuboidal epithelia. • It may show calcification. |
Usual Ductal Hyperplasia It is a benign process with a heterogeneous cell population of variable size and shapes with areas of nuclear overlapping; it can be either • Mild UDH: 2-4 cell layer in thickness, • Florid UDH: more extensive changes Both types have no luminal bridging, which is often observed among atypical ductal hyperplasia. |
[8] |
|
Apocrine metaplasia • The glands are rounded, of variable-sized vesicular nuclei and prominent nucleoli, lined with cells showing abundant granular, eosinophilic cytoplasm • Glands may exhibit apical luminal sniffing, and secretions, which may calcify Apocrine metaplasia may be either cystic or papillary configuration |
Adenosis A benign process defined by acinar cell proliferation, it can be either • Nodular adenosis has a discrete nodule shape • Sclerosing adenosis: fibrous tissue will compress and surround the proliferated glands, making acin' distorted and can mimic the shape of invasive carcinoma |
[9, 10] |
2.3. Therapeutic Approach
Provides a comprehensive critique of all available options, their mechanisms of action, advantages, limitations, and supporting references, which encompass:
•Lifestyle changes
•Supplements and nutrients
•Pharmacological drugs, including both hormonal and non-hormonal treatments
•Innovative therapies
3. UNDERSTANDING PATHOLOGICAL CHANGES
Fibrocystic Breast Changes are primarily of two types, either proliferative or non-proliferative; the differences in both are summarized in Table 1. It should be noted that both types often present together in the same patient, and they may be focal to one area or diffusely distributed [7].
4. CLINICAL PRESENTATION AND FINDINGS ON EXAMINATION
On examination, tenderness and increased nodularity are noted, and the breast may feel like a “bag of peas.” In some cases, palpable cysts may be present. Integrating clinical findings, biopsy (when indicated), and imaging is crucial for the accurate diagnosis and management of breast lesions, including FBC. [11, 12]
5. IMAGING MODALITY FOR FCB DIAGNOSIS
Advancements in imaging have revolutionized diagnosis and management options in breast diseases, including FBC [14].
Since the 1960s, mammography has evolved as a key tool in managing diseases, complementing clinical examination and biopsy. Fig. (5) for normal mammography and Fig. (6) for mammography of FBC. Later, ultrasound (introduced in the 1970s–1980s) was performed. Fig. (7) shows a breast ultrasound with a typical FBC. In the 1990s, MRI was introduced, further improving diagnostic accuracy and helping to exclude unnecessary biopsies [15]. Table 2 summarizes the key aspects of each imaging modality used for FBC. Imaging plays a vital role in patient screening, guiding breast biopsies, and confirming definitive histological diagnoses. Moreover, its significance extends beyond diagnosis, as it is essential for patient follow-up and ongoing therapeutic planning [16]. By enabling the tracking of fibrocystic breast changes (FBC) over time, clinicians can monitor FBC progression and regression, facilitating informed decision-making and improving patient outcomes.
5.1. Recent Advancements in Breast Imaging
There were giant leaps in breast imaging during the last decade, which include:
5.1.1. 3D Mammography (Digital Breast Tomosynthesis)
This technique (DBT) involves taking multiple low doses of mammography of the breast from multiple angles to be reconstructed again in a 3-dimensional model. It has the advantage of superior breast disease diagnosis, including FBC, compared to the standard 2-dimensional mammography; thus, it helped reduce false results and unnecessary biopsy [23].
5.1.2. Contrast-enhanced Mammography (CEM)
This technique involved the admission of iodine-based contrast media before imaging. Enhanced contrast highlights refer to areas with high blood flow, such as FBC. This method had higher sensitivity and specificity, even in dense breast tissue, compared to standard mammography (Fig. 8) [24].
5.1.3. Advances in Breast Ultrasound Imaging
Breast ultrasound has evolved in terms of imaging quality and the emergence of newer techniques. One is elastography, which assesses tissue stiffness as a crucial variable in discriminating between benign and malignant conditions. The other is automated breast ultrasound, which allows comprehensive breast tissue assessment. It is capable of diagnosing architectural distortion, has a superior diagnostic performance to the standard ultrasound, and is in agreement with MRI in assessing tumors. Both modalities have improved ultrasound accuracy in breast diseases, including FBC [25, 26].
| Aspect | Mammography | Ultrasound | MRI | Ref. |
|---|---|---|---|---|
| Role in everyday practice | • It allowed for the first time a non-invasive detection of FCB. • Currently, it is the cornerstone of breast imaging. |
• Complementary to mammograph., • It is of particular benefit in suspicious mass evaluation and dense breast tissue. |
• Primarily used for high-risk cases and specific clinical scenarios, with family risk. • Limited for FBC. |
[17, 18] |
| Points of Strength in FBC Breast Imaging | • There is increased breast density. • The appearance can be quite diverse, from well-circumscribed densities to ill-defined areas with microcalcifications manifested as tea-cup low-density lesions in multiple lobes. • Can spot cysts, calcification, and architectural distortion. |
• Characteristic FBC pattern: multicyclic area associated with well-circumscribed anechoic lesions; may be solid on occasion, representing fibrous tissue. • Guides breast intervention as fine-needle aspiration. |
• FBC appeared as hyperintense cysts on the T2 weighted image, while fibrous tissue is shown as a low signal on the T1 and T2 weighted image. • It has a limited role in FBC since they do not have distinctive features. • Particular benefit in invasive carcinoma |
[19] |
| Pros & cons of each Technique in FBC | • High sensitivity and specificity for detecting and evaluating FBC. • It misses subtle changes, especially dense breast. |
• It is inferior to mammography. • Efficient in defining mammographic abnormalities and differentiating solid from cystic. • Especially helpful for young cases and with dense breasts. |
• Limited role in the routine assessment of FBC. • In high-risk conditions, it is extremely sensitive and can diagnose subtle lesions. |
[20] |
| Pros & cons of each Technique in general | • There is radiation exposure • Not expensive |
• No radiation exposure • Inexpensive and it is operator-dependent. |
• No radiation exposure. It uses a magnetic field. • It is expensive and time-consuming. • If used with contrast, it may cause claustrophobia |
[21, 22] |
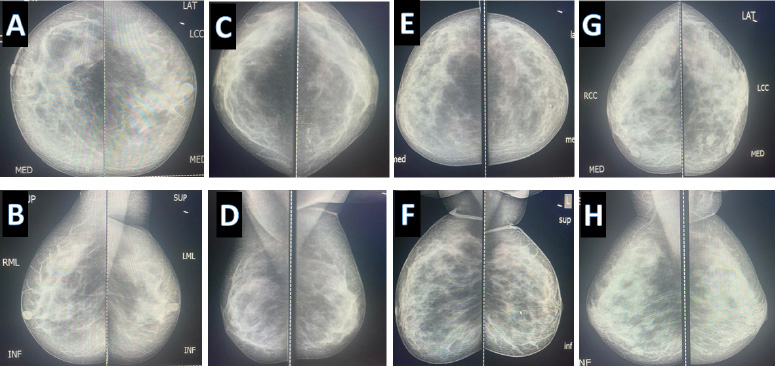
Wide diversity of “normal mammography” (A, B) same patient in craniocaudal and Mediolateral oblique view respectively, same applies to (C, D, E, F), and (G, H).
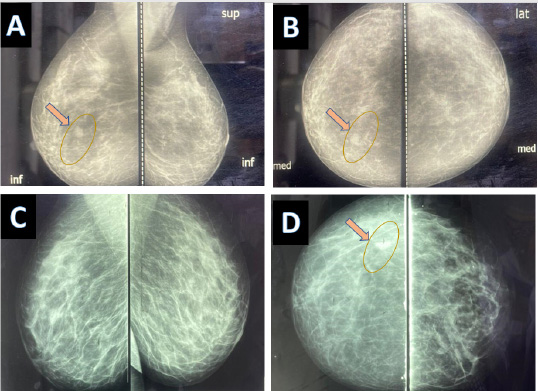
(A, B) Mammography of 27 years old lady with fibrocystic changes of the breast, a small cyst is observed on the medial aspect of the breast (C, D) Mammography of a 43 years old lady with fibrocystic changes of the breast, a small cyst is observed on the lateral aspect of the breast.
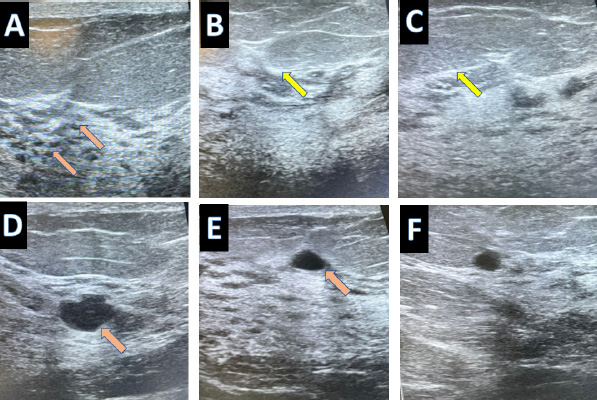
Typical fibrocystic changes in breast tissue in a 25-year-old female, (A) with abundant cystic changes (B, C) fibrous tissue bands (D, E, F), prominent thin wall ducts, and multiple small cystic changes
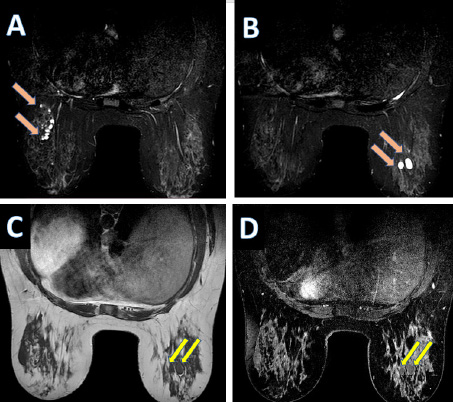
Contrast-enhanced breast MRI of a 45-year-old female present with mastalgia. (A & B) axial T2 SPAIR, (C) axial T1, (D) axial T1 post contrast administration show moderate background enhancement, and there are multiple scattered parenchymal cysts showing no enhancement.
5.1.4. Contrast-enhanced Breast MRI (CE-MRI)
As mentioned earlier, the MRI role in FBC is limited, but adding contrast helped distinguish behaviors of potentially malignant cases. Therefore, this method is reserved for undetermined or complex lesions caused by other diagnostic modalities [27].
5.1.5. AI-assisted Technique (Mammography, ultrasound, and MRI)
Similar to several areas of medicine, radiology has integrated artificial intelligence (AI), with algorithms developed to assist radiologists in improving diagnostic accuracy, including for FBC, and in identifying subtle changes that may be underestimated by humans. The results have shown promising outcomes in cancer detection and a reduction in false-positive results. However, research in this field is ongoing and requires further development [28].
5.1.6. AI-powered Computer-aided Diagnosis (CAD)
In addition to AI integration in imaging modalities, there is evolving research on comprehensive AI-powered computer-aided diagnosis, which receives input data from many sources and is processed simultaneously, adding more reliable and holistic patient screening. One of the most reliable deep learning models was convolutional neural networks. It showed a remarkable ability to detect and localize breast lesions to efficiently guide radiologists in spotting suspicious lesions [29, 30]. The rapid progress and evolution of imaging have significantly enhanced the future of breast disease imaging, particularly for FBC.
5.2. Limitations and Challenges of Breast Imaging
The precision and accuracy of imaging in FBC can be hindered by more than one factor. To begin with, there are operator factors that lead to inter-observer variations. The experienced radiologist is most likely to spot minor or subtle changes and to position the patient to optimize the quality of obtained images [17, 31].
Patient-related factors exist, as cases with dense breast tissue may be missed by mammography. Some cases may be asymptomatic, which makes managing decisions challenging. In contrast, cases with severe pain may encounter difficulty in taking the ideal imaging position, in addition to stress and fear of any abnormal finding. Consequently, the patients' communication and cooperation may become challenging [32]. Finally, device-related factors also play a role, as each imaging modality has its limitations, and inadequate resolution may obscure the diagnosis. Sometimes, there is a variation in imaging protocols across different centers, impairing the result consistency. Finally, restricted access to advanced imaging can hinder a comprehensive assessment of the case [33, 34]. Addressing those challenges and limitations in FBC imaging can significantly enhance diagnostic accuracy, optimize patient follow-up, and improve overall outcomes.
5.3. Role of Imaging in Differentiation of FBC and Brest Cancer
It is not unusual for cases with FBC to be presented with breast mass or nipple discharge added to the usual premenstrual pain. The overlapped clinical picture of FBC with breast cancer symptoms can be quite distressing [10].
The shared similarity, coupled with the globally rising incidence of breast cancer and the widespread awareness of its symptoms, often leads to fear and anxiety among women. Even a benign finding may raise concerns about malignancy [1]. A careful clinical examination is necessary, as FBC presents with tender, lumpy breasts. These lumps are typically multiple, mobile, and non-fixed [1, 11].
In contrast, cases with breast cancer usually present with a solitary hard, non-mobile lump that is usually accompanied by skin and nipple changes. Imaging has an indispensable role; it may confirm or exclude cancer and, in suspected cases, can guide biopsy to confirm the definitive diagnosis [7].
The value of each imaging modality in FBC versus breast cancer is summarized in Table 3. With ultrasound guidance, fine needle aspiration can help differentiate between the two. In FBC, aspiration typically retrieves clear or cloudy fluid, whereas in breast cancer, it may yield cellular material that reveals malignant cells.
6. THERAPEUTIC MODALITIES FOR MASTALGIA IN FCB
To have a deeper insight into how to address mastalgia, we need to understand mastalgia in FCB. Mastalgia may coincide with FCB but can be seen isolated as part of normal hormonal fluctuation during menstruation [35]. During the menstrual cycle, hormonal fluctuation (estrogen and progesterone) affects the breast tissue and causes fluid retention [36]. Another cause for mastalgia is increased breast sensitivity owing to estrogen dominance on breast tissue. The increased fibrous tissue noted among FCB cases will trigger nerve endings by compromising them and contributing to higher pain levels [37]. Elevated prolactin levels also contribute to increased breast sensitivity and fluid retention [38]. Moderate-severe pain among affected cases can be addressed by targeted therapy and keeping a personalized approach for each case. It included lifestyle changes and medical and surgical options added to innovative therapeutic approaches.
6.1. Lifestyle Changes
Lifestyle changes are commonly used as the first line of treatment and include:
Wearing a supportive bra is highly recommended, as it reduces mastalgia by minimizing unwanted movement, alleviating pain and strain on sensitive tissues, and providing immediate comfort and relief [39].
Some recommend reducing caffeine intake, which, when taken in excess, causes extra nervous system stimulation and thus reduces the pain threshold for the breast tissue. However, the supporting evidence regarding this topic is mixed and inconclusive [40].
Reduced dietary intake of fat, particularly saturated fat, tends to reduce estrogen production, thereby reducing estrogen dominance and stimulation. This approach showed mild-moderate efficacy in some cases [41]. Increasing dietary fibers tends to increase estrogen excretion in the GIT tract, leading to normalizing blood estrogen and reducing stimulation of breast cells; it can be used as part of holistic management in FCB therapy [42].
6.2. Medical Modalities in Treating FCB-related Mastalgia
The medical modalities include supplements and vitamins, traditional Chinese herbs, and drugs (non-hormonal and hormonal), as shown in Fig. (9).
6.2.1. The Use of Vitamins and Supplements in FCB-related Mastalgia
Many studies have examined the use of vitamins and dietary supplements alone or in combination. The most commonly used types, their mechanisms of action in alleviating mastalgia, efficacy, and side effects are summarized in Table 4.
Using vitamins such as (E and B6) effectively reduced mastalgia. The B6 vitamin was considered the first option due to its availability and lower cost [43].
Adding Omea-3, a fatty acid to vitamin E, did not outweigh vitamin E alone in relieving mastalgia [44]. Despite its effectiveness in alleviating mastalgia, flaxseed oil did not outperform vitamin E when used as monotherapy [45]. Both vitamin B6 and evening primrose oil capsules demonstrated comparable efficacy in reducing mastalgia, particularly cyclical mastalgia [43]. An evaluation of diet and supplements showed promising results in reducing pain, swelling, and breast nodularity while improving quality of life (QOL) [46,47]. Probiotics are live microorganisms that promote a healthy gut flora balance when consumed in adequate amounts [48]. They are essential in supporting gut health, immune function, and many aspects of human health, including hormonal regulation [49]. In 2021, they were tested in FCB. They had a significant impact on reducing mastalgia, in addition to reducing blood inflammatory markers and promoting a healthy life [50].
| Imaging Type | Fibrocystic Changes | Breast Cancer | Ref. |
|---|---|---|---|
| Mammography | • Increased breast tissue density, an abundance of fibrous tissue, and multiple cystic lesions may be filled with fluid. | • A breast mass with a poorly defined irregular edge. Calcification may be evident as well. | [20, 21] |
| Ultrasound | • Well-defined and echoic cysts with well-demarcated borders | • Ill-defined hypoechoic mass with occasional post-acoustic shadowing | [22] |
| MRI (Magnetic Resonance Imaging) | • It shows areas of enhancement, suggesting benign changes | • Suggestive signs of an aggressive process include rapid enhancement& wash-out pattern | [23, 24, 26] |
Medical modalities in treating FCB-related mastalgia.
The encouraging results given by these supplements are hindered by variability in response and the complexity of mastalgia management. Further research is warranted to underscore genetic, racial, and hormonal factors that cause different responses to treatment. Moreover, there is scarce data on the long-term effect and optimal dose. More comprehensive studies are necessary to compare these supplements or combine them with other therapeutic options like non-steroidal anti-inflammatory drugs (NSAIDs) to establish the best therapeutic option.
| Vitamins and Supplements | Suggested Action | Efficacy in FCB | Side Effects | Refs. |
|---|---|---|---|---|
| Vitamin E | It shows anti-inflammatory and anti-oxidant activity, thus reducing pain | Supporting evidence is inconsistent; it had a mild effect on pain and is mainly used by those seeking natural treatment. | Fatigue and headache. May interfere with anticoagulants | [51] |
| Vitamin B6 (Pyridoxin) | It reduces elevated prolactin levels, which helps alleviate mastalgia, making it suitable for managing hormonally induced pain. | Supporting evidence is not strong; some may get the benefit | Overdosing can cause neuropathy. | [52] |
| Vitamin D | It is an anti-inflammatory, hormonal modulator that reducesthe estrogen domain thereby reducing cellular proliferation in the breast. | Efficacy is mild to moderate. It reduces pain by reducing inflammation and normalization of hormonal levels. | Overdosing can cause hypercalcemia and GIT upset. | [53] |
| Magnesium | It improves muscle relaxation and reduces water retention in the breast | Evidence suggests mild-moderate efficacy. It is mainly used for premenstrual symptoms. | Overdosing can lead to abdominal cramps and electrolyte imbalance | [54] |
| Iodine | It alters estrogen metabolism and promotes healthy breast architecture | Mostly considered when the pain is hormonal in origin, efficacy not well confirmed | Over or under-dosing may affect TH | [55] |
| Evening prime rose oil capsule. | Gamma-linolenic acid normalizes prolactin and thus reduces tenderness. | Inconsistency in results some improve, and some do not, widely used alone or in conjunction with others | GIT symptoms and headaches are not advised for those with seizures | [56] |
| Omega 3-fatty acids | It exerts anti-inflammatory activity, reducing mastalgia and breast pain | It is popularly used to relieve pain of mild-moderate severity | GIT upset may interfere with anticoagulant therapy | [44] |
| Probiotic | Anti-inflammatory and anti-oxidant action, thus reducing mastalgia | It was effective in reducing pain and added to the reduction of associated depression symptoms | Minimal | [50] |
| Flaxseed | Phytoestrogens regulate estrogen levels and reduce mastalgia | Widely used as natural hormonal support, however, supporting evidence is not strong | Mild GIT symptoms | [57] |
| Polyphenols | A bioactive compound in olive m green tea has anti-inflammatory and anti-oxidant action and is in growing pain. | Via modulation of estrogen effect on the breast, it reduces mastalgia; it is a promising supplement but needs further validation. | Overdosing can cause GIT upset. | [58] |
| Melatonin | A dietary supplement and a hormone showing anti-oxidant action and reducing estrogen domain in the breast may regulate hormonal disbalance. | Efficacy in reducing mastalgia was limited, and it was not significant. | Mild headache and dizziness | [59] |
6.2.2. Traditional Chinese Medicine (TCM) in FCB-related Mastalgia
These are traditional herbs that are commonly used in practice, and one of them is FCB. The most common and popular are chaste berry and turmeric; both are scientifically supported and are recommended in Western herbal practice [60].
The white peony and licorice combination is popular in traditional Chinese medicine and recognized in Western practice for its hormonal properties. Less common herbs valued and appreciated in Chinese traditional medicine are Dong Quai, Xia Ku Cao, and Chai Hu; these herbs are used alone or in combination with other groups. Table 5 illustrates the popular TCM with suggested benefits, efficacy, and side effects in FCB [61].
There are many gaps in the use of Chinese herbs, including the unclear underlying mechanisms, unidentified active ingredients, and lack of standardized dosages. Additionally, long-term safety data are insufficient, highlighting the need for large-scale randomized controlled trials. The integration of traditional Chinese medicine (TCM) into Western therapies warrants further exploration [62].
6.2.3. Non-hormonal Drug Therapy in FCB-related Mastalgia
Many drugs were implemented to reduce mastalgia and show diverse efficacy. Some of the non-hormonal therapies are not suitable for long-term therapy due to their side effects [35]—the complexity of mastalgia urges for combination or using a non-pharmacological approach. The latter may address more than one aspect of FCB and show few side effects. Some of the drugs used, such as gabapentin and metformin, are not suitable for everybody and are given in special indications. In Table 6, a summary of non-hormonal therapies, their mechanism of action, and side effects are summarized.
| Herb | Suggested Mechanism of Action | Efficacy and Use in FBC of the Breast | Side Effects | Refs. |
|---|---|---|---|---|
| Chasteberry (Vitex agnus-castus) | Normalizes hormonal levels, especially for prolactin, reducing mastalgia and tenderness | Good efficacy in reducing mastalgia | Dizziness, nausea, skin rash | [63] |
| Turmeric / Curcumin (Curcuma longa) | It exhibits powerful antioxidant and anti-inflammatory properties, reducing inflammation and tenderness. | Often used for its efficacy in reducing pain and inflammation added to overall breast health. | Some reported GIT symptoms, and it may interact with blood thinners. | [64] |
| White Peony and Licorice Combination | It normalizes the hormone effect on the breast tissue, reducing estrogen predominance. | A common herb in traditional Chinese medicine, it relieves hormonal pain. | Overdosing may increase blood pressure in some cases. | [65] |
| Peony (Paeonia lactiflora) | It has a unique hormonal balancing effect on females; thus, it promotes menstrual and breast health. | It is often combined with other herbs because it has moderate efficacy in reducing pain and normalizing hormonal levels. | It has a minimal effect, however, it is not advised for cases with hepatic illness. | [66] |
| Dong Quai (Angelica sinensis) (female ginseng) |
It maintains estrogen balance, and it addresses menstrual symptoms | It is often combined with other herbs because it has moderate efficacy in reducing pain and normalization of hormonal levels | Trivial, including GIT symptoms, not for pregnant nor cases of blood thinners | [67] |
| Chai Hu (Bupleurum) | It prevents stress-related hormonal imbalance | It has low efficacy and is used as part of an herb mix to relieve mastalgia | Trivial, including GIT symptoms; however, not recommended for cases & and those on blood thinners | [68] |
| Drug Name | Mechanism of Action | Efficacy and Popularity in Practice | Side Effects | Refs. |
|---|---|---|---|---|
| Analgesia | ||||
| Acetaminophen | Suppresses pain signals to the brain | Commonly used for mild-moderate pain | Only overdosing can cause hepatic toxicity. | [37] |
| - | Non-steroidal anti-inflammatory drugs | - | ||
| Ibuprofen, Naproxen (systemic) |
It inhibits Cyclooxygenase(COX), thus lowering PG, leading to reduced inflammation and pain levels. | Commonly used for mild-moderate pain, it limits inflammation | Prolonged use causes gastric upset | [35] |
| Diclofenac Gel (local) |
It inhibits COX, thus lowering PG, leading to reduced inflammation and pain levels in the site applied. | Popularly and effectively in local relief of pain | Local skin irritation while systemic Effects are reduced | [69] |
| - | Diuretics | - | ||
| Spironolactone | It alleviates breast swelling and tenderness by reducing fluid retention | It is used on occasion, especially for premenstrual tension | Dizziness and electrolyte imbalance | [70] |
| - | Selective Serotonin Reuptake Inhibitors (SSRIs) | - | ||
| Fluoxetine, Sertraline | Mainly used for PMS as it indirectly reduces mastalgia via serotonin level adjustment dysphoria syndrome. | Occasionaly prescribed with some effectiveness for cyclic mastalgia. Supporting evidence is weak. | Nausea, headaches, mode changes | [71] |
| - | Neuromodulator | - | ||
| Gabapentin | It has limited use, designed originally for neuropathic pain, and helps to alleviate pain caused by nerve entrapment. | Not routinely prescribed, it helps cases with nerve entrapment. | Dizziness and drowsiness occur and should be monitored under supervision. | [72] |
| - | Biguanide | - | ||
| Metformin | It reduces insulin sensitivity, has an ant-inflammatory Effect, reduces hepatic neogenesis, Reduced hyperglycemia dampens estrogen production and prolactin, leading to reduced breast tissue stimulation. |
It is not a common treatment for FCB, but it has benefits in cases with insulin resistance and PCOS. It exerts anti-inflammatory action and regulates insulin, estrogen, and prolactin hormones, thereby reducing mastalgia. | Common side effects: GI issues (nausea, diarrhea), severe but rare: lactic acidosis (especially with renal impairment). | [73] |
6.2.4. Hormonal Drug Treatment in FCB-related Mastalgia
This category contains a wide range of drugs that are effectively used to suppress breast pain [74]. It has a targeted mechanism of action, some of which are suppressing ovulation and reducing estrogen excess, as in oral contraceptive pills (OCCP). Others, such as Tamoxifen, show effects on the estrogen receptor and block them from suppressing unwanted estrogen stimulation. Danazol, a steroid with antiandrogenic activity, is known for its undesirable effect on prolonged use, so it is not recommended for prolonged use [75, 76]. Some of the hormones are not routinely used unless there is an inappropriate level, as in thyroid hormones and dopamine agonists [77,78].
A common issue with hormonal drugs is that symptoms may recur after discontinuation of treatment. Some cases may not respond, particularly if the pain is due to non-hormonal causes. These drugs can also interact with metabolic diseases such as diabetes and hypertension (DM and HT), making them unsuitable for all patients. Future research should concentrate on newer and safer hormonal drugs and explore the best combination with other non-hormonal or innovative approaches in management. Table 7 illustrates the hormonal drugs used in managing FCB, including their mechanism of reducing pain, benefits, efficacy, and side effects.
6.3. Innovative approach for FCB-related Mastalgia
Innovative therapy in Treating FCB-related mastalgia has evolved, aiming for effective relief of pain and discomfort. These approaches showed promise in enhancing patient satisfaction and reducing side effectsas shown Table 8. Fibrocystic breast changes still impose therapeutic challenges, and for that, these innovative strategies offer promising perspectives for more effective treatment and targeted approaches.
| Drugs Category; Composition | Mechanism of Action | Modality of Reducing Pain | Efficacy | Side Effects | Refs. |
|---|---|---|---|---|---|
| Oral Contraceptives (OC) | Combined pills contain estrogen and progesterone | Reducing estrogen dominance and establishing hormonal balance thus alleviating mastalgia | It reduces mastalgia and breast tenderness. | Moo swings, headaches, weight gain, nausea, not safe for smokers, and metabolic diseases | [75] |
| Nextstellis 4th generation OCCP |
Estetrol (3mg) has SERM activity. Drospirenone (15mg) a synthetic progesterone with anti-androgen & and mineral- corticoid |
Estetrol manages hormonal fluctuations, and drospirenone tends to reduce fluid retention at the breast, thus reducing pain and swelling | Effective for mastalgia and is gaining popularity due to fewer adverse effects on clot and breast cancer risk | Estrogenic and androgenic side effects are less compared to other OCCPs. | [79] |
| Synthetic progestogen ; Progestin |
Medrogestone (1st generation) and dydrogesterone(2nd generation) | By mimicking natural progesterone, they balance hormones and dampen estrogen dominance in breast | Effective or mastalgia, mastopathy, and breast soreness | Well tolerable, especially among cases with low progesterone | [6] |
| Natural Progesterone ; Micronized progesterone |
Progestogel® (transdermal progesterone gel) | It normalizes estrogen levels, thus reducing proliferative activity on breast tissue, and by reducing cellular permeability, it reduces cycle size and number. | Very effective and sustainable relief of mastalgia, especially if used throughout the period | The local application reduces systemic side effects, and it is well-tolerable | [80] |
| Danazol | A synthetic steroid with androgenic properties | Dampens estrogen production by suppressing ovarian function, with a net reduction of the size of breast cysts and associated mastalgia. | Useful for pain and cyst reduction, especially among severe cases | Mood swings, weight gain, androgenic side effect | [76] |
| Selective estrogen receptor modulator (SERM) | Tamoxifen | It blocks the breast receptors for estrogen, which reduces cyst formation and humpers estrogen dominance. | It is effective in reducing pain among severe cases | Mood swings, hot flushes and nausea. However, it can increase blood clots | [81] |
| Ormeloxifene | It blocks the breast receptors for estrogen, which reduces cyst formation and humpers estrogen dominance. | Effectively reduced pain scale and reduced breast nodularity. It was superior to danazol. | Headache, nausea, delayed menses | [82] | |
| Dopamine agonists that inhibit prolactin secretion | Bromocriptine, Cabergoline | By lowering prolactin levels, it reduces associated mastalgia | Effective in cases where prolactin is increased | Fatigue, dizziness, nausea. It can affect the heart valve (Cabergoline) | [78] |
| Other Dopamine agonists | Lisuride (used in Parkinson's) Quinagolide (selective agonist of Dopamine receptor) |
Lisuride reduces prolactin and associated mastalgia Quinagolide normalizes hormonal levels and reduces pain and tenderness |
Effective in cases where prolactin is increased | Headache and dizziness | [83, 84] |
| Complete estrogen blockade via a Combination of centchroman(SERM) &Gosereline (LHRH analogue) |
Centchroman & Gosereline | By reducing estrogen levels and blocking its receptors in the breast, they relieve refractory mastalgia and reduce tenderness. | Very effective and sustainable relief of mastalgia; it reduced pain scale when 1st line therapy failed. | Acceptable and minor | [85] |
| Thyroid hormones | (Levothyroxine) | By normalization of TH levels, the estrogen levels are corrected. It eventually reduces mastalgia by establishing hormonal balance. | It is of value for cases with TH imbalance, but it needs monitoring | If incorrect dosing, the patient may have hypertoxicosis symptoms | [77] |
| Method | Mechanism of Action | Supporting Evidence | Benefit among Patients | Refs. |
|---|---|---|---|---|
| Physical approaches | ||||
| Physical therapy, as manual therapy, massage and stretching exercise | Improves oxygenation to the tissue and enhances blood supply and lymphatic drainage, which positively reduces muscle tension | The supporting evidence indicates increased oxygen levels in the area following exercise, along with reduced tissue hyperplasia and associated symptoms. This approach has been successfully applied in cases of chronic mastalgia. | It can be an adjuvant therapy to other treatments or used as a preventive approach for chronic mastalgia. | [86] |
| Acupuncture | Applying pressure to specific anatomical sites reduces stress and promotes relaxation, in addition to blocking the transmission of pain signals to the brain. Stimulation of acupuncture points triggers the release of natural opioids (endorphins) by the brain. | It regulates estrogen secretion and effectively improves blood flow by reducing the resistance index. | It was effective in reducing pain in cases of cyclical mastalgia, such as in fibrocystic breast disease and breast cancer-related pain. | [87] |
| Transcutaneous Electrical Nerve Stimulation | Using low-voltage electrical currents to inhibit pain signals to the brain | It improved the pain scale felt, reduced the anxiety of chronic pain, and gave women a sense of control over their pain. | It was effectively used in cases of mastalgia post-breast cancer surveillance; it has potential in FCB, but evidence is still lacking. | [88] |
| Cryoablation | The ultrasound-guided extreme cold was applied to reduce breast cysts | The evidence in FCB is encouraging but needs further work, and it was successfully used in breast fibroadenomas and cancer | It was effective in reducing the size of breast cysts and reducing pain triggered by cyst pressure both in benign and malignant cases. It was of good safety and had few side effects. | [89, 90] |
| Low-Level Laser Therapy (LLLT) | By laser, we reduce tissue inflammation and health. | It is used to show promising results in other breast conditions. Further work is needed to support its use in FCB. | It was effective in reducing the size of breast cysts and alleviating pain caused by cyst pressure in both benign and malignant cases. It demonstrated good safety and was associated with few side effects. | [91] |
| Mental Health Approaches | ||||
| Cognitive Behavioral Therapy Mindfulness Meditation and yoga |
It changes patients' perspective on chronic pain and helps them adopt coping strategies. | The evidence of its benefit in cases with fibromyalgia is strong. | It changes patients' perspective on chronic pain and helps them adopt coping strategies. | [37, 92, 93] |
| Virtual reality | It acts by distracting pain perception in addition to modulating how the body reacts to pain. | Evidence during the intervention, coping with pain, and during the course of therapy was proven. | It was successfully used in breast cancer cases, during biopsy procedures, and throughout the course of chemotherapy. The evidence in fibrocystic breast conditions supports its efficacy. | [94] |
| Music | Interfers with pain perception and activity of CNS neurons. Enhances tolerability of pain and modifies pain intensity |
Widely implemented among breast cancer patients post-surgery, either alone or combined with exercise. Reduces tension and lowers anxiety levels |
Complementary tool to reduce pain scale, enhance effective coping, and improve QOL. | [95, 96] |
| Cognitive Behavioral Therapy Mindfulness Meditation And yoga |
It changes patients' perspective on chronic pain and helps them adopt coping strategies. | The evidence of its benefit in cases with fibromyalgia is strong. | It changes patients' perspective on chronic pain and helps them adopt coping strategies. | [37, 92] |
| Virtual reality | It functions by distracting pain perception and modulating the body's response to pain | Evidence during the intervention, coping with pain, and during the course of therapy was proven. | It was successfully used in breast cancer cases, during biopsy procedures, and throughout the course of chemotherapy. The evidence in fibrocystic breast conditions supports its efficacy. | [94] |
| Music | It interferes with pain perception and the activity of central nervous system neurons, enhances pain tolerability, and modifies pain intensity | Widely implemented among breast cancer patients post-surgery, either alone or combined with exercise. Reduces tension and lowers anxiety levels |
It serves as a complementary tool to reduce pain intensity, enhance effective coping mechanisms, and improve quality of life | [95, 96] |
6.4. Surgical approach for FCB-related Mastalgia
Fine needle aspiration relieves pain caused by large cysts and excludes malignancy in suspicious lesions [97].
Surgery is indicated when cysts do not respond to pain medication or are refilled quickly. Surgery is also indicated if imaging studies or cytology suggest suspicious features. Cysts tend to recur and are often removed to improve patient QOL [98].
7. PROGNOSIS AND FOLLOW-UP
Proliferative-type fibrocystic breast changes increase the risk of breast cancer by one to two times in both breasts. The presence of ductal changes or calcifications necessitates a six-month follow-up, with the risk of breast cancer rising up to five timesThe updated guideline many agencies advocate is a personalized follow-up based on personal risks and imaging results, so the “1-size fits all model” is no longer applicable [99].
8. INNOVATIVE AREA IN RESEARCH
Bioinformatics has evolved many aspects of breast disease diagnosis, including breast cancer and fibrocystic breast changes (Fig. 10) [100-102].
These innovative tools(including machine learning and AI) allowed multi-data integration and led to the discovery of newer biomarkers [103, 104].
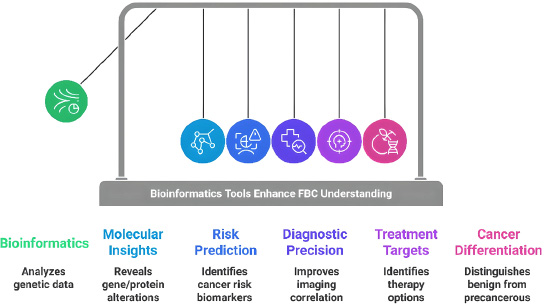
The key roles of bioinformatics in breast disease.
The latter improves diagnostic precision, enabling earlier detection of malignancies and differentiation from benign cases such as fibrocystic changes [105]. Additionally, biomarkers can unveil the pathology that leads to disease progression; thus, it can lead to newer therapeutic strategies [106]. We must acknowledge the limitations of traditional diagnostic methods; being invasive is the most frequently reported, which innovative diagnostic strategies may overcome. However, these techniques should be tested and validated before they can be applied in practice [107]. Indeed, bioinformatics and AI open newer diagnostic and therapeutic avenues that improve overall patient outcomes [108].
CONCLUSION
Breast imaging is a pivotal tool for diagnosing, managing, and following fibrocystic breast (FBC) cases. Mammography takes the lead in diagnosis, while ultrasound is complementary and aids in dense tissue examination. MRI is not for routine use but is recommended for suspicious and high-risk cases. Future studies are warranted to explore how to integrate emerging technologies, validate their role, and establish and standardize imaging protocols to improve imaging protocols' effectiveness in FBC management and follow-up.
This research finding emphasizes that lifestyle modification remains the first-line approach, complemented by pharmacological interventions tailored to the patient's pain type and etiology.For the majority of cases with FCB, lifestyle changes added to medical therapy are the preferred strategy in treatment; surgery is preserved for severe, recurrent, and suspicious cases.
Innovative treatment approaches showed optimistic results, minimal side effects, good efficacy, and high patient tolerability. Future studies should aim to identify the optimal combination of therapies, appropriate dosing, and duration, while also exploring novel strategies to enhance patient satisfaction. Optimizing the management of fibrocystic changes will mitigate its negative impact on women's quality of life and improve patient outcomes.
AUTHORS' CONTRIBUTIONS
The authors confirm their contribution to the paper as follows: M.A.G.Z.: Data Analysis or Interpretation; S.K.A.: Methodology; R.J.: Visualization; W.N.M.H.: Draft manuscript. Author. All authors reviewed the results and approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| FBC | = Fibrocystic breast change |
| DBT | = Digital Breast Tomosynthesis |
| CEM | = Contrast Enhanced Mammography |
| CAD | = Computer Aided Diagnosis |
| TCM | = Traditional Chinese Medicine |
| RCTs | = Randomized Controlled Trials |
| COX | = Cyclooxygenase |
| PG | = Prostaglandins |
| OCCP | = Oral Contraceptives |
| LLLT | = Low Level Laser Therapy |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The protocol was approved by the Mustansiriyah Ethics Committee of Obstetrics and Gynecology/Iraq (NO: 47) on 7/8/ 2024.
CONSENT FOR PUBLICATION
The patient provided signed consent for the publication of the photograph and the data related to her case.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information are available within the article.
ACKNOWLEDGEMENTS
The authors would like to thank Mustansiriyah University, Iraq for its continuous support.


